-
How is the implant fixed to the bone?
By a biological process called osseointegration, in which the body forms a direct connection between the bone and the implant surface. Following osseointegration, the implant becomes firmly fixed to the bone and can support a prosthesis capable of dealing with all functional and cosmetic requirements as though it were a natural healthy tooth.
-
When is the right time to have an implant?
1. When one has to replace teeth with an equal or greater stability to that of the natural teeth that were lost, while avoiding having to use adjacent teeth; to restore the mouth functionally and cosmetically with quality and precision.
2. When one needs an anchor for a mobile dental prosthesis, to provide the necessary stability for comfort and security, as though it were a fixed prosthesis.
3. When one needs the maxillary bones to maintain their function and not lose volume because of reabsorption, avoiding tissue deterioration and the aspect of facial ageing caused by the formation of folds and creases.
4. When anchors are needed to allow other treatments such as orthodontics or orthopaedics and that might, on occasion, be impossible to perform.
-
How can one deal with the absence of an isolated tooth?
Using a dental implant, we can recover the loss of a natural tooth without having to use or file down the adjacent healthy teeth (however, this would be inevitable if one opts to introduce a bridge to support the teeth), Over the implant, we fashion a unitary or independent crown which can be cemented or fixed to the implant using a small hidden screw. In this way, the crown will have a totally natural appearance with totally restored phonation and chewing functionality without needing any support from neighbouring teeth.
-
How can one recover a series of lost teeth?
When one has lost various teeth and the space is relatively small, they can be recovered by introducing a fixed prosthesis called a bridge, which can be supported by ones natural teeth. If you wish to avoid filing down the natural teeth, it is advisable to introduce a set of implants in the space that can support the bridge instead. Nowadays, implants are the best option; no natural teeth are affected when supporting the prosthesis and the teeth are not overloaded. In addition, the bone volume and the soft tissue remain intact.
-
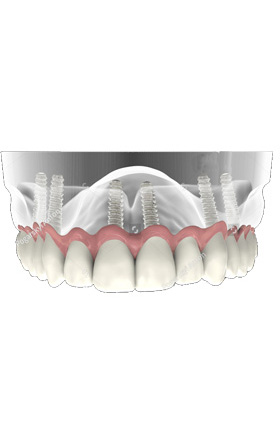
How can one restore the mouth when there are no teeth at all?
Mouth reconstruction in people who have lost all their teeth can be performed by introducing a complete prosthesis. However, there are certain drawbacks:
1. Loss of stability, adjustability and retention that can cause movement, difficulty in chewing and instability.
2. Slow but continuous reabsorption of the maxillary alveolar bone.
3. Sores in areas where there is friction.
4. Loss of appetite and changes in food flavours.
5. In some patients, it can produce nausea. By fixing various dental implants, we can fit a stable prosthesis, improving comfort and stability. A fixed prosthesis can be used (only taken out by the dentist) or a denture (that the patient can remove themselves), which ensures great stability when it is in place.
-
Is dental implant treatment painful?
We almost always administer a local anaesthetic, as with many other dental treatments. One only hears the gentle noise of the instrument and a mild pressure sensation. After the operation, there might be some inflammation in the affected area and bruising. This is completely normal, a natural response to repair tissue after the intervention. Our implantation team will advise you on the best treatment, and help you to avoid any discomfort after the implants have been fitted.
-
Can the implants be fitted immediately after the teeth have been removed, or should I wait?
This depends on the reason for the tooth loss. In cases where infection is present, it is advisable to wait until the bone tissue returns to normal; otherwise, the reliability of the treatment might be compromised. If no infection exists, we can fix the implants during the same session.
-
How do I care for my mouth during the osseointegration period following implant placement?
Some of the factors that can affect the osseointegration process are:
1. Infection. Those patients who do not practise sufficient mouth hygiene and, above all, those who have periodontal disease, run a higher risk of bacterial contamination of the implants.
2. Loading on the implants: often, too much force applied on the implants can interfere with the normal integration process between the implant and the bone.
3. Smoking: smokers run a higher risk of complications since the toxic elements in tobacco affect the normal osseointegration process. Most of the complications following dental implant treatment occur with these patients.
-
When might I need special surgical procedures?
Although in most cases the implants carried out follow the procedure described above, occasionally cases arise in which the quality or quantity of either the bone or the gum requires techniques especially directed at remedying the problem. These procedures, based on using grafts, try to increase the gum quantity and quality in the intervention area to make implants possible.
-
What does the maintenance phase consist of?
Implant-based treatments have proven themselves to be very safe and secure. This is because of the existence of exhaustive control and maintenance protocols. Establishing adequate vigilance and careful periodic maintenance is necessary to avoid both bacterial infection and any possible maladjustments of the prosthesis caused by wear and tear over the passage of time. Check-ups aim to control the treatment results over time by detecting any undesired situations and rectifying them early.